In those with an autoimmune condition, the immune system produces antibodies that end up attacking the body's own tissues instead of fighting infections in response to an unknown trigger. There are over 80 types of autoimmune diseases categorized primarily by the different area(s) of the body that they affect (e.g., psoriasis, rheumatoid arthritis, and inflammatory bowel disease).
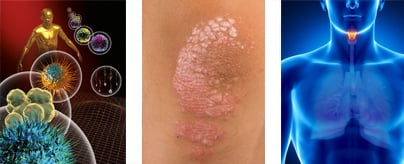
It is estimated that autoimmune diseases affect roughly 5-10% of the world's population, and this may be underestimated. Most (about 75%) diagnosed with autoimmune disease are women.
The symptoms of autoimmune disease depend on the specific category of autoimmune disease one may have, but may include:
The consequences of allowing autoimmune disease to progress uncontrolled range from life-threatening to a minor inconvenience, depending on the category and organs involved.
No one is certain what causes autoimmune disease, although there are some clues to guide us. Genetics seems to play a role in who may be more likely to develop an autoimmune disease, however, when populations migrate from an undeveloped country to a Westernized country, for example, their risk of developing an autoimmune disease goes up, suggesting a clear environmental link. Investigators are considering a number of possible environmental links such as diet, toxin exposure, and intestinal bacteria imbalance.
Dr. Fuhrman’s general supplement protocol for adults (see Vitamin Advisor for details) includes:
Multivitamin (without beta-carotene, vitamin A, vitamin E, folic acid, copper), such as Women’s Daily Formula +D3, Men’s Daily Formula +D3, or Gentle Care Formula.
Omega-3 DHA and EPA, such as DHA+EPA Purity.
Optional: Consider adding a mixed mushroom immune supplement, such as Immune Biotect, because of the potential immune system benefits throughout life from assorted mushroom phytochemicals that are not normally consumed in the diet. Consult your physician if you are on medication.
For supplement recommendations personalized to you, your health condition and goals, visit the Personalized Vitamin Advisor and answer a few questions.
Sign up for the online Combat Autoimmune Disease and Cancer Masterclass
Supervised, periodic water fasting can be used as an adjunct treatment for autoimmune conditions. I have documented remission of autoimmune diseases following supervised fasting in a published series of case reports.35 Additional studies have found that fasting (followed by a vegetarian diet) reduces pain in rheumatoid arthritis patients.36,37 Continuing to follow a Nutritarian diet after completing the fast is essential for sustaining the benefits of the fast. Fasting puts the body into a repair mode, facilitating the elimination of damaged molecules, reducing inflammation, and resetting the immune system.38,39 I generally recommend that patients adopt the dietary protocol for a few months prior to considering adding fasting to their protocol. Fasting is not compatible with most medications.
Fasting should be done under the supervision of a competent health professional.
ONLINE: All members of DrFuhrman.com can search the Ask the Doctor archives for discussions on this topic. Platinum and Diamond members can connect with Dr. Fuhrman by posting questions in the forum. Not a member? Join now.
IN PERSON or ONLINE: Book a consultation with a specialist at Longevity Rx in San Diego, California, run by Joel Fuhrman, MD and Cara Fuhrman, ND. Using nutritional protocols, cutting-edge screening tools, advanced imaging, and innovative treatments for pain and injuries, they'll create a personalized action plan to help you prevent and recover from illness, and achieve your optimal weight. Book online at Longevity Rx or call +1 (858) 367-3558
EVENTS: Join Dr. Fuhrman for an online boot camp, detox or other event. During these immersive online events, you’ll attend zoom lectures, follow a special meal plan, and have access to a special, live Q&A session with Dr. Fuhrman. Learn more about events.
The following are sample questions from the Ask the Doctor Community Platinum and higher members can post their health questions directly to Dr. Fuhrman. (All members can browse questions and answers.)
I have recently been given a preliminary diagnosis of multiple sclerosis. My symptoms are relatively mild, mostly numb areas and tight or spasmodic muscles, sometimes a little dizziness. I have been on your basic Eat for Health plan for about 10 weeks now.
I recently read and implemented your autoimmune protocol. Because I have such mild symptoms, I had hoped that I would have seen a halt to new symptoms by now. I know that nerves take a long time to heal so am resigned to living with the old symptoms for a while but thought that new numb spots and/or tight or spasmodic muscles would not be forming by now.
Follow the autoimmune protocol carefully and continue to eliminate gluten and casein indefinitely. Make sure you get your 25 hydroxy-vitamin D level checked and supplement to get your level in the high end of the optimal range (30 -50ng/ml). Vitamin D is a potent immune modulator. A study in JAMA found a dramatically lowered risk of MS in individuals with the higher vitamin D levels. Also, get out into the sun. Recent evidence suggests that UV light is doing something beyond vitamin D to reduce risk. You can take up to 5 grams of EPA/DHA per day, but make sure the purified fish oil has more EPA than DHA. Add curcumin to your diet.
There are many great recipes in the Recipe Guide within the Member Center. Spend time reviewing them.
It is important to give this time. Just stick with it, and try to reduce your stress about it. There is good evidence that the central nervous system can repair itself, so be hopeful.
I have RA and have followed the autoimmune protocol 100% for 4 months now. The results came slow, but are impressive. Sed rate is back to normal, very little pain, medication greatly reduced. Hopefully I’ll be a success story sometime soon. There was a recent bump in my journey. In the past 4 months, I ate tomatoes every day and eggplant once or twice a week (and never noticed any problems); but in the last 2 weeks I added potatoes (with skin) and mini-Mexican bell peppers almost every day. MY PAIN WENT UP for the first time! This leads me to the following questions:
Is nightshade avoidance a must for RA? Maybe I just had an overload of nightshades, is this possible? What should I do to test for nightshade intolerance?
I agree with you. You overdid the nightshades and paid a price. Avoid them for the next few weeks then only have small amounts. About 20 percent of RA patients are nightshade sensitive. Many with nightshade sensitivity can still tolerate a small amount, but when they go overboard they can get into trouble.
What are the common food allergens/sensitivities for someone with RA who follows a nutritarian vegan diet? From my clinical experience I found: Gluten, nightshades (about 20% of patients, based on prior thread), citrus, nuts, corn (rare), beans (rare).
Your thoughts (adds/deletes) would be appreciated. Thanks.
I don’t think nuts are a common sensitivity in RA patients. That would be pretty rare too. Too much fruit in general is usually not advised as some are just somewhat fructose sensitive. Rarely some are sensitive to beans, and even though mostly Lupus patients are sensitive to sprouts (especially alfalfa sprouts), some people with RA do not do well with sprouts either.
I have had minor joint pain for the past two years. Seven days ago, after taking hydrocodone for some oral surgery pain, all my joints began to really hurt. I immediately went on the autoimmune protocol. I have a CRP and anti-CCP blood test scheduled for tomorrow, after which I plan to fast for 7-10 days. Unfortunately, in the last week, several small nodules have appeared on my knuckles. My sister (who has RA) thinks I should get right on the methotrexate to prevent further joint damage. I’m not sure what to do since the nodules are forming even though I’m following the protocol exactly. What do you think?
That is great you are tackling this with nutrition and not with highly-toxic drugs that cause cancer. Drugs should be the last resort treatment, not the first. This works for the broad majority of individuals, but it can take a few months. The nodules and inflammation can improve. Incorporating fasting as you are planning usually speeds up the benefits. Keep me posted with your progress and blood test results. This sounds more like osteoarthritis and not rheumatoid, so that is not as severe a condition, however it can take longer to see benefits from dietary excellence.
My mother has suffered from rheumatoid arthritis for many years; she is 78 years old and the disease has advanced significantly. She has been on medications to treat the condition and has experienced significant disfiguration in her hand/feet joints. That said, about 6+ months ago I converted her to a vegan diet, and she has experienced significant weight loss and an improvement in her general biomarkers. I was thinking it might be a good idea to put her on Dr. Fuhrman’s multivitamin for women, fish oil supplements, and a probiotic to help her out.
A vegan diet is usually very helpful, but you should review my autoimmune protocol in my book, Super Immunity. A nutritarian diet specifically targets immune system repair that can make the dietary protocol even more effective. Not all patients with RA respond exactly alike. Some benefit from limiting certain fruits, wheat, or beans. Others are fish oil responsive and benefit from higher amounts that others do not. If she has no medical contraindication to high dose fish oil, she can give it a trial for a few months and track if it helps. I usually recommend about 4,000-6,000 mg of a high EPA content fish oil daily–make sure it is purified, so free of contaminants. Likewise, probiotics are helpful for some and not others. She can use the one we carry here in double the typically recommended dose, and test it for a few months on and off to see if it has a positive effect. My women’s multivitamin assures that various essential nutrients are present that could be relatively low in one’s diet. With RA it is particularly important to make sure no deficiencies exist in zinc, B12 or Vitamin D.
I know that you have had substantial success in assisting patients with psoriasis. What I am trying to unravel is whether you take a targeted approach in your prescriptions. Within the general framework of a nutritarian diet, are there certain foods that a person with psoriasis should avoid? In addition, are there certain types of foods (and nutrients) that you recommend a person with psoriasis should consume, and in what quantities? In this context, are there any supplements which you recommend? Is fasting recommended? I strongly suspect there’s a relationship between diet and my psoriasis, but I’m not sure I have the will power for a radical change, however, my psoriasis now is worse than it has ever been -- widespread and very itchy at times -- and I have to tackle it.
It does not take much will-power; it takes knowledge. Once you have the knowledge it seems pretty foolish to suffer with psoriasis. Did you read my book, Super Immunity and the position papers stressing the high-green diet for psoriasis? When you are really committed to get rid of your psoriasis, let me know. You are correct to assume it will necessitate a radical change in your diet. You will have to cut out animal products, coffee, other drinks, and the processed sweets. The mistake you are making is that you think you can't give up your food addictions and won’t enjoy eating a diet without all those compromises. It will take more work, and I know change is stressful, but once you eat this way for a few months you will enjoy it just as much and lose your desire for all the low nutrient junk you are eating. You just have to do it, and you may be surprised that it is easier and tastier than you think. Your fear and hesitation in changing is not based on fact but an emotional response to change.
In the past year I fell off the nutritarian diet and am now trying to once again get psoriasis under control. You had told me in the past that if I gained back the weight the psoriasis would come back. This time it is back with a vengeance and the arthritis too. I am very motivated to change, especially after reading articles on the links between psoriasis and heart attack/stroke risk.
How should I get started...Vitamix? Medicine? Supplements? Gym membership?
I do not wish to lose the use of any more joints and want to stop the inflammation ASAP.
The place to start is 100 percent dietary perfection with no compromises and no excuses (and to exercise every day, no matter what the weather). Instead of medications, juice fast a few days and water fast a few days to curtail inflammation every few weeks. Follow the dietary protocol for autoimmune disease from my Super Immunity book. You do not have to have a gym membership to exercise vigorously. The most important supplement to assure adequacy is Vitamin D. Do not let yourself get deficient in that.
Can pustular psoriasis be reversed with a nutritarian diet? I developed this disease about 8 years ago. I currently eat a SAD diet, I’m about 50 pounds overweight, smoke a few cigarettes a day, and I don’t exercise. I take Soriatane for it. My dad also had it. I’m skeptical that diet will help since I think mine is one of the worst forms of psoriasis and is probably hereditary. I’m currently on antibiotics and steroids for walking pneumonia. I have a terrible cough and am wheezing and out of breath, and my doctors suspect maybe allergies or asthma or perhaps a reaction to my meds are the cause.
Genetics plays a lesser role in all forms of psoriasis (and autoimmune disease in general), but early life environmental and dietary factors are the major contributory factors in those susceptible individuals. Smoking, obesity, and alcohol have been shown to increase the severity of the disease. Infections and exposure to antibiotics can also worsen the course. It takes a strongly motivated person to heal their body via nutritional excellence, and you have multiple addictions going on, so you have to take the initiative to learn more so you have the tools and education to change. Reading my book Super Immunity would be a good start. You would have to be willing to give up cigarettes cold turkey and simultaneously give up your old diet. It is not impossible; I have seen people do it. It might be helpful for you to be seen in the office, since it sounds like you have complex issues and could use the extra motivation. If you follow the protocol carefully, lose weight, and stop smoking, you should benefit greatly.
The autoimmune protocol lists dietary avoidance of salt, wheat, and oil as one of the guidelines. I have psoriasis and have been following this protocol. Currently I avoid wheat and gluten. Is it only wheat that needs to be avoided or all grains with gluten?
You can still eat low gluten grains, such as oatmeal, but most do better with avoiding wheat, rye, and barley.
I have been suffering with seborrheic dermatitis (or psoriasis) on my scalp and in my ears for about 10 years now. I have gone to many dermatologists and have tried every treatment there is, including lotions, creams, different shampoos, etc. I have also tried some natural soaps, shampoos, essential oils, probiotics, etc.
Nothing has really helped. It is very frustrating because I have dandruff, and it looks terrible and it constantly itches. My ears have a white dry layer that shows the minute I stop using the medicated cream.
Do you think this can be eradicated by following a nutritarian diet? Are there any topical products or supplements that might help? Since I would be doing the protocol for skin related issues and not digestion problems, would I avoid oatmeal and all grains, beans, sweet potatoes, and nuts? If so, what do you suggest as energy sources? My confusion comes from not being positive which foods definitely cause the problem.
You should review my autoimmune guidelines in my book, Super Immunity. We frequently see people with psoriasis improve with the autoimmune protocol outlined there. The key features are a strict ETL vegan diet, high dose EPA/DHA (omega 3 fatty acids), no wheat, no dairy, supplemental flora (probiotic), supplemental vitamin D (if levels are low), minimal dried fruit, large salad or blended salads, and a glass of fresh vegetable juice per day. The digestive track is what promotes the immune dysfunction that causes the attack on your skin, which is why the probiotic is often helpful. This protocol eliminates the most likely allergens and is high in the phytonutrients that will heal your immune system. Eat raw nuts and seeds like walnuts, cashews, and sunflower and sesame seeds along with the foods listed in the autoimmune position paper. Start with avoiding gluten for six weeks and any other food that you feel you may be sensitive to.
You need to follow the protocol 100 percent, not 95 percent, to get better, and even then it could take months to see improvement. No snacking on nuts and seeds, just some with the salad or in the salad dressing. Since you relate that your problem is severe, it may be best to have a comprehensive evaluation in our office, with blood work.
Suffering the debilitating effects of lupus and multiple autoimmune diseases made Lynsey's life miserable; now with her 65 pound weight loss her life has a new vibrancy... Read More
Results may vary.

Janet lost 102 pounds, has stopped taking steroids for multiple sclerosis and feels better than she has for the last two decades... Read More
Results may vary.

Linda lost 72 pounds; is off all medications and has more energy then ever despite having multiple sclerosis... Read More
Results may vary.

Joyce is free of daily rheumatism flare-ups... Read More
Results may vary.

Theresa's Rheumatoid Arthritis has almost disappeared along with her 52 pound weight loss... Read More
Results may vary.

Todd's arthritis pain is much better without having to take the toxic drug his doctor had prescribed and he lost 58 pounds... Read More
Results may vary.

Sharon lost 42 pounds; her lupus numbers are in normal range and she has more engergy than ever... Read More
Results may vary.

Karen suffered severe side effects from her Rheumatoid Arthritis medications; now she is free of RA symptoms and meds... Read More
Results may vary.

Jane lost 30 pounds, is free of psoriasis and stopped taking blood pressure medication... Read More
Results may vary.

After years of suffering Jodi now controls her painful psoriasis and other autoimmune diseases... Read More
Results may vary.