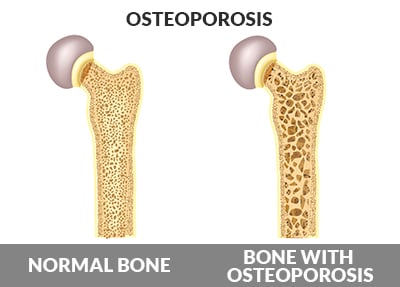
Osteoporosis is a state in which the bones are thinner, more porous, and therefore, are at increased risk of fracture.
Statistically, women older than 60 years old have a lifetime risk of a bone fracture of 44% (25% for men), and for those with osteoporosis, this risk goes up to 65% (42% for men).1 If you have osteoporosis, you likely wouldn’t know it as it doesn’t cause any specific symptoms in most people. A bone density measurement is helpful at determining where you fall on the bell curve of the average person’s bone density. The World Health Organization (WHO) decided that if your bone density is worse than the average young adult by 2.5 standard deviations, then you have osteoporosis. The reality is that it is a continuum (not a sharp line) and risk of fracture goes up as your bone density gets worse. Getting lower bone density is, in part, a natural consequence of inactivity and weak muscles and is also typical of normal women after menopause. The problem comes when this progresses from acceptable, low fracture-risk levels to high fracture-risk levels, which can lead to a hip fracture, which is associated with higher morbidity and mortality mostly due to prolonged care needed in hospitals and nursing homes and being bedridden afterwards (blood clots, pneumonia, urinary tract infections, bedsores, etc.). The more chronic diseases we have before getting a fracture at an older age, the worse the outcome (higher risk of death). Remember that weak bones is only one risk factor, and other risk factors contribute to a fall that results in a fracture. Factors that increase risk of bone fractures include:
So, the best strategy is a combined approach of maximizing the required nutrients from healthy eating and supplementation (which also reduces chronic disease risk over the years), and exercising to help keep the muscles and bones strong, minimizing fall risk as well as fracture risk.
A Nutritarian eating style will provide a broad spectrum of nutrients required for strong bones including potassium, calcium, vitamin K, magnesium, vitamin C, and others. Here are some of the foods high in calcium (as well as vitamin K, magnesium, potassium, and vitamin C) to include in your mix of food choices:
Plant foods in general have a higher absorption rate of calcium than supplements and dairy products, and calcium is best absorbed by eating moderate to high calcium plants foods at each of your meals throughout the day.
Avoid supplemental vitamin A, caffeine, excessive salt, excessive animal product intake, and soda (all lead to excessive calcium loss).
For supplement recommendations personalized to you, your health condition and goals, visit the Personalized Vitamin Advisor and answer a few questions.
Regular exercise to strengthen the back and hips is the priority as these areas tend to be the most common for fractures in those with osteoporosis. Here are a few examples of exercises that you can include in your regular workouts to strengthen your back and leg bones:
Members can review my video, Osteoporosis Protection For Life, for more information and a comprehensive exercise plan.
Reid IR. Cardiovascular effects of calcium supplements. Nutrients 2013, 5:2522-2529.
Greendale GA, Salem GJ, Young JT, et al. A randomized trial of weighted vest use in ambulatory older adults: strength, performance, and quality of life outcomes. J Am Geriatr Soc 2000, 48:305-311.
Greendale GA, Hirsch SH, Hahn TJ. The effect of a weighted vest on perceived health status and bone density in older persons. Qual Life Res 1993, 2:141-152.
Shaw JM, Snow CM. Weighted vest exercise improves indices of fall risk in older women. J Gerontol A Biol Sci Med Sci 1998, 53:M53-58.
Snow CM, Shaw JM, Winters KM, Witzke KA. Long-term exercise using weighted vests prevents hip bone loss in postmenopausal women. J Gerontol A Biol Sci Med Sci 2000, 55:M489-491.
The following are sample questions from the Ask the Doctor Community Platinum and higher members can post their health questions directly to Dr. Fuhrman. (All members can browse questions and answers.)
Will a healthy person eating a Nutritarian diet be able to stop the progression of osteoporosis or simply slow the bone loss?
Weight-bearing exercise combined with a Nutritarian diet (high in green vegetables, fruits, nuts, seeds, and legumes, and low in animal protein) is the most reliable way to increase bone strength and maintain bone health throughout our lives. Even if you already have osteoporosis, as you follow a high-nutrient eating style and build your muscle strength through exercise, it is possible that you may both prevent progression of the disease and also see an increase in bone mass. Natural plant foods are rich in important bone-building nutrients like calcium, magnesium, and vitamin K1; vitamin D is an important supplement to take. Find out your level of 25-hydroxyvitamin D and supplement based on the results to reach the range of 30-45 ng/ml. Some women may also benefit from a small amount of supplemental calcium (see the Vitamin Advisor for details).
Remember, exercise is the key to strengthening bone and maintaining favorable bone health with aging. Muscles and bones get stronger in tandem. Read this article to learn more about bone-building exercise and the best and worst foods for bone health.
If I am out of shape, where do I start regarding building muscles and strengthening bones to prevent osteoporosis? The only exercise I currently do is to walk a few times per week. I do not have access to a gym or any exercise equipment at home. Are there any effective, basic exercises I can do?
Also, can a Nutritarian diet reverse early osteoporosis?
Walking is not sufficient to prevent osteoporosis of the back. If you are limited and inexperienced in exercise, it will be helpful for you to purchase a weighted vest that you can wear for a few hours each day. You should also walk up and down the stairs in your home. My DVD, Osteoporosis Protection for Life, contains the information you are looking for. There I show you the most effective bone-building exercises that you can do without equipment, almost anywhere.
Progression of osteoporosis can be significantly slowed and even reversed when you combine a Nutritarian diet with the right type of exercise and vitamin D sufficiency. As you build your level of fitness and strength through exercise and increase muscle strength, it is possible to not merely prevent the progression of osteoporosis, but also see an increase in bone mass.