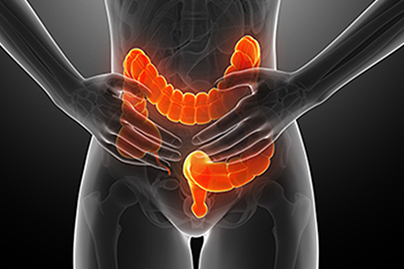
Ulcerative colitis (UC) is a chronic inflammatory disease in the family of inflammatory bowel diseases (IBD) that causes inflammation and damage to the large intestine and/or rectum.
Ulcerative colitis (UC) is more common in Western and Industrialized countries and seems to be increasing in developing countries as they adopt Western habits, such as poor diet. Approximately 0.2% of the U.S. population suffers from UC.1
Some of the potential explanations of this geographical trend include Westernized factors, such as antibiotic use, hygiene, exposures to certain infections, pollution, and diet. A higher risk follows those with a family history of the disease as well. Intestinal permeability (leaky gut) and altered intestinal bacteria seem to play an important role, but it is still not known exactly what causes UC.
Those with UC may experience some or all of the following symptoms:
Nutrition plays a key role to help those with UC. Improvements in lower inflammation and intestinal bacterial balance precede improvements in symptoms, and even remission is possible.
Dr. Fuhrman’s general supplement protocol for adults (see Vitamin Advisor for details) includes:
Multivitamin (without beta-carotene, vitamin A, vitamin E, folic acid, copper), such as Women’s Daily Formula +D3, Men’s Daily Formula +D3, or Gentle Care Formula.
Omega-3 DHA and EPA, such as DHA+EPA Purity.
Optional: Consider adding a mixed mushroom immune supplement, such as Immune Biotect, because of the potential immune system benefits throughout life from assorted mushroom phytochemicals not normally consumed in the diet.
Additional supplements:
Probiotics: UC and Crohn’s disease are both associated with alterations in the gut microbiome that are thought to be involved in the disease process.12 Studies suggest probiotics may be helpful for promoting remission in ulcerative colitis.13 Eating foods rich in fiber and resistant starch also helps to maintain a healthy gut microbiome.
Omega-3 fatty acids: High-dose DHA and EPA have anti-inflammatory effects that may be beneficial in Crohn’s disease.14,15 Talk to your doctor to find out if high-dose omega-3s are appropriate for you.
Curcumin: Curcumin, a collection of phytochemicals from turmeric, has anti-inflammatory effects. Limited evidence suggests curcumin supplements help to maintain remission in ulcerative colitis.16,17
ONLINE: All members of DrFuhrman.com can search the Ask the Doctor archives for discussions on this topic. Platinum and Diamond members can connect with Dr. Fuhrman by posting questions in the forum. Not a member? Join now.
IN PERSON: Book a stay at Dr. Fuhrman’s Eat to Live Retreat in San Diego, California. With options ranging from one, two and three months (and sometimes longer) you will be under Dr. Fuhrman’s direct medical supervision as you hit the “reset” button on your health. For more information: (949) 432-6295 or [email protected].
EVENTS: Join Dr. Fuhrman for an online boot camp, detox or other event. During these immersive online events, you’ll attend zoom lectures, follow a special meal plan, and have access to a special, live Q&A session with Dr. Fuhrman. Learn more about events.
The following are sample questions from the Ask the Doctor Community Platinum and higher members can post their health questions directly to Dr. Fuhrman. (All members can browse questions and answers.)
I’ve been diagnosed with a mild form of ulcerative colitis. Hoping for a long-term solution to control this problem, I started your IBD protocol four days ago (I am only eating the foods listed in Phase 1, as noted in the March 2008 newsletter No 36 and taking all the recommended supplements) and was wondering about what to expect in terms of symptom reduction.
My current symptoms are blood and mucus with stool. How long should I expect to be on Phase 1 before the bleeding stops? Do I also need to wait for the mucus to stop completely before moving to Phase 2? In Phase 2, it says tofu can be added. Can beans be added then as well? When can whole grains (brown rice, quinoa, millet) be added back in?
It usually takes about 3 months to bring micronutrients in the body’s tissues to a high enough level to reduce the inflammatory response. Juicing speeds up this process. It sounds like your condition is not so severe, so the likelihood of a recovery via nutrition is high.
After a few weeks of phase one, beans can be added, but only start with a small amount for the first week and then increase very gradually. I would stick with brown rice, wild rice, quinoa, and millet and not add back wheat for a few months, until you are considerably better. Make sure you are taking the supplements with probiotics, Vitamin D, and fish oil too.
I suffer from ulcerative colitis. The diet I am trying to heal with is:
Green smoothies without fruit; Dr. Fuhrman’s soup recipes, fully blended; homemade soft white bread; oatmeal; maybe a banana; some melon or a peach
What do you think? Will this diet help me heal?
First you have to review my protocol for ulcerative colitis that I describe in more depth in my newsletter on inflammatory bowel disease. The supplemental protocol is important too. You have to avoid the white bread, and in fact, it would be best to avoid all gluten grains. Make sure you’re having steamed kale, collards, and bok choy, along with steamed asparagus, squash, avocado, carrots, peas, artichokes, and mushrooms. Include some tofu or tempeh a few times a week. Doing this will reduce inflammation and provide the protective phytonutrients that are critical to heal your gut. Continue to have blended salads without fruit. Steam all the greens, including leafy greens, before blending in your smoothie, and add steamed zucchini to the smoothie. Raw fruits and vegetables can be irritating for a person with bloody ulcerations, and I like to keep the diet mostly cooked until the bleeding stops, and then, slowly introduce small amounts of soft lettuce and other raw food gradually.